What you need to know about breast cancer
By The Cure Cancer Team | Updated 8 October 2025
Self-exams, screening eligibility in Australia and what you can do after you've been diagnosed. This article is for general awareness only and is not a substitute for medical advice. Please speak with your GP about your personal circumstances.

Breast cancer is the most common cancer affecting women and people assigned female at birth globally, with nearly 20,000 new cases diagnosed annually in Australia alone. Early detection significantly improves the chances of successful treatment and survival, which is why it’s so important to learn how to perform a self-exam for breast cancer and to understand other preventive measures.
Additionally, knowing what questions to ask your doctor if you are concerned about breast cancer, or if you receive a breast cancer diagnosis, can empower you to make informed decisions about your health.
How to perform a self-exam for breast cancer

Be breast aware: get to know the normal look and feel of your breasts as part of everyday life. If you notice a change, see your GP. You don’t need a special technique or a set schedule.
1. Visual inspection
Stand in front of a mirror with your arms resting against your sides.
Look at your breasts in the mirror and check for any visible changes such as dimpling, puckering, changes in shape, size, or symmetry, or changes in the nipple or areola.
2. Feel your breasts while lying down
Lying down on your back, use the pads of your fingers to examine the entire breast. Start from top to bottom and side to side, then from the collarbone to the top of the abdomen, and finally from the armpit to the cleavage.
Follow a pattern to ensure that you cover the whole breast. You can choose a circular motion, vertical lines, or a wedge pattern (starting at the nipple and moving outwards).
3. Feel your breasts while standing or sitting
Follow the same motion as above, covering the entire breast and armpit area. You might find it easiest to do this whilst in the shower.
4. Know what to look for
- Lumps, thickening or hard knots
- Swelling, warmth, redness, or darkening
- Change in size or shape
- Dimpling or puckering of the skin
- Itchy, scaly sore or rash on the nipple
- Nipple discharge
The importance of breast cancer research

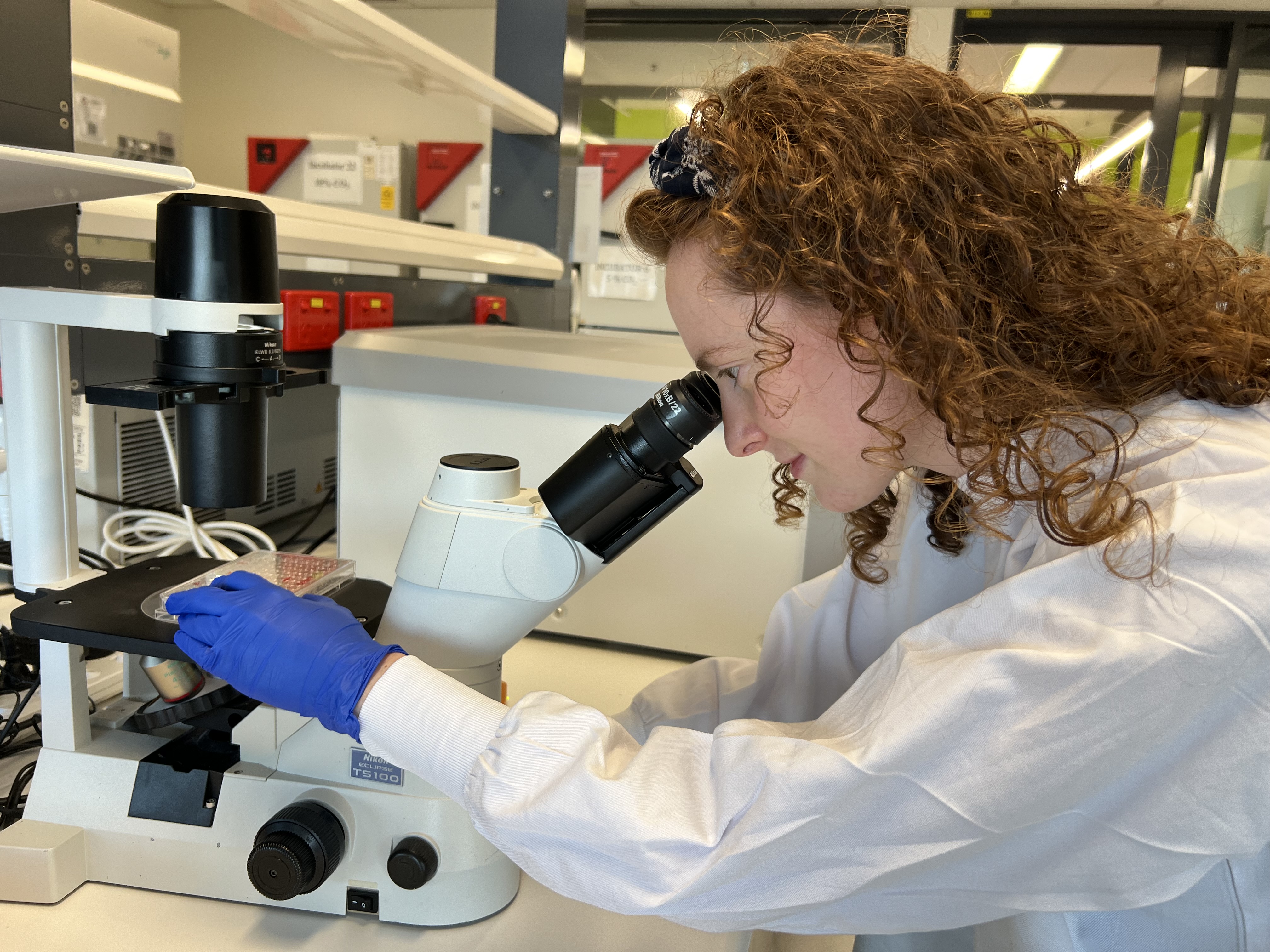
2024 Cure Cancer-funded breast cancer researcher Dr Kellie Mouchemore.
Cure Cancer is proud to have backed over 60 innovative breast cancer research projects, all of which have contributed to significant advancements in understanding, detecting, and treating the disease. Thanks to research, the 5-year relative survival for breast cancer has increased from 77% to 92% between 1989 to 2018. Research efforts have improved early detection methods, developed more effective treatments, and increased survival rates.
By investing in groundbreaking research, Cure Cancer-funded scientists can continue to:
- Develop new treatments: Research helps identify new drugs and treatment methods, offering hope to those with difficult-to-treat breast cancer types.
- Improve early detection: Early detection is key to increasing survival rates.
- Increase understanding of risk factors: Research helps identify genetic, environmental, and lifestyle factors that increase breast cancer risk, allowing for better prevention strategies.
- Enhance quality of life: Research also aims to improve the quality of life for breast cancer survivors by managing side effects and developing supportive care practices.
Understanding how to perform a breast self-exam, taking preventive measures such as routine screenings, maintaining an open dialogue with your GP, and supporting cancer research are all essential steps that contribute to reducing the impact of breast cancer.
Find out more about the breast cancer projects we’re currently funding and make a donation here.
Breast cancer screening: Know your eligibility

In Australia, cisgender and transgender women aged 40 and over can access free mammograms every two years. The highest risk group is women aged 50-74, who are routinely invited to screen every two years. Regardless of gender identity, anyone registered as 'female' with Medicare aged 50-74 will receive screening invitations. Source: BreastScreen Australia Program.
It is important to note that Aboriginal and/or Torres Strait Islander women are routinely invited and recommended to screen from age 40.
Although women aged 40-49 (excluding First Nations women) and those over 74 can access screening, they won’t receive regular invitations. If you fall into these groups or aren’t registered as ‘female’ with Medicare, it’s important to be proactive—consider booking your mammogram or GP appointment to stay on top of your breast health.
Here is a breakdown of your eligibility for breast cancer screening via the BreastScreen Australia Program:
Cisgender and transgender
women
- Aged 50-74 or from age 40 if Aboriginal and/or Torres Strait Islander: Eligible for free mammograms every 2 years; routinely invited to screen.
- Aged 40-49 and 75+: Eligible for free mammograms every 2 years, but not routinely invited.
- Trans women on hormones for 5+ years aged 50-74 or from age 40 if Aboriginal and/or Torres Strait Islander: Eligible for free mammograms every 2 years; routinely invited if registered as 'female' with Medicare.
Trans men and gender diverse people
- Trans men and gender diverse people assigned female at birth (AFAB) who have not undergone gender-affirming top surgery: Recommended to screen every 2 years starting from age 50-74, or from age 40 if Aboriginal and/or Torres Strait Islander.
- Gender diverse people assigned male at birth (AMAB) on hormones for 5+ years: Advised to screen every 2 years starting from age 50-74, or from age 40 if Aboriginal and/or Torres Strait Islander.
Family history of breast cancer / BRCA1 or BRCA2 gene mutations
- Consult your doctor about starting individual routine screenings earlier.
- High-risk individuals may need additional imaging tests such as MRIs.
Under 40
- Not eligible: you’re not eligible for BreastScreen. Be breast aware and see your GP promptly if you notice any breast changes.
- Breast cancer can occur in women and AFAB individuals under 40. Talk to your doctor if you have a family history of breast cancer or any concerns.
Not registered as 'female' with Medicare
- If eligible, be proactive in booking a screening mammogram.
- Although rare, breast cancer can occur in cisgender men and AMAB individuals. Be aware of the symptoms and talk to your GP if you notice anything unusual.
Partial mastectomy / Top surgery
- Discuss personal risk factors with your doctor, considering family history, hormone treatments, and previous surgeries.

Trans women and gender diverse individuals assigned male at birth (AMAB) who have been on gender-affirming feminising hormones for 5+ years are advised to screen every 2 years from ages 50-74 or from age 40 if Aboriginal and/or Torres Strait Islander.
Trans men and gender diverse individuals assigned female at birth (AFAB) who have not undergone gender-affirming top surgery are advised to have screenings every two years, from ages 50-74, or from age 40 if Aboriginal and/or Torres Strait Islander. For more information on breast screening for trans and gender diverse people, ACON offers a valuable online resource called 'Can We'. You can also check your eligibility here.
People with a family history of breast cancer or who carry the BRCA1 or BRCA2 gene mutations can talk to their doctors about starting individual routine screenings earlier if they are under 40. High-risk individuals may also need additional imaging tests, such as MRIs. Those who have had a partial or double mastectomy, or gender-affirming top surgery, should also discuss their personal risk factors with their doctors, with consideration for family history, hormone treatments, and previous surgeries.
Men and breast cancer

While breast cancer is much rarer in cisgender men and AMAB individuals, it can still occur. Around 200 people assigned male at birth are diagnosed with breast cancer each year in Australia (source: Cancer Australia). Cisgender men and AMAB individuals should be aware of breast cancer symptoms, such as lumps or changes in the breast area, and talk to their doctor if they notice anything unusual.
Trans men who have undergone gender-affirming top surgery should consider speaking to their doctor about their individual breast cancer risk.
If you discover any changes during a self-exam or have concerns about breast cancer, it’s important to consult with your doctor. Here are some questions to guide your conversation:
- What type of screening tests are available to me?
- Am I considered high-risk for breast cancer?
- What lifestyle changes can I make to reduce my risk of breast cancer?
After a breast cancer diagnosis

Receiving a breast cancer diagnosis can feel overwhelming and confusing. It’s helpful to bring a notebook or have a friend or family member with you to take notes during your appointments. Being well-prepared and informed will help you feel more in control and make the most informed decisions for your health. Consider asking:
- What type and stage of breast cancer do I have, and what does that mean for my prognosis?
- What additional tests do I need, and what are my treatment options?
- What are the potential benefits, risks, and side effects of each treatment option?
- How will the treatment affect my daily life, long-term health, fertility, and quality of life?
- What support services and resources are available to help me during treatment and recovery?