World Cancer Research Day 2023: 6 brilliant cancer research breakthroughs
By Sylvia Lee | 23 August 2023
In the lead up to World Cancer Research Day on 24 September, Cure Cancer is celebrating our funded researchers’ incredible achievements.

Dr Arutha Kulasinghe's cellular atlas of skin cancer showing the epidermal layer in blue and glands near the surface.
World Cancer Research Day recognises the huge gains we have made in cancer research throughout the history of modern medicine, and the work ahead of us that still needs to be done to improve cancer screening, diagnosis, treatment, survivorship, and palliative care.
As a leading cause of death worldwide, cancer causes at least 10 million deaths every year, placing significant physical, emotional, psychological, and financial strain on patients, families, communities, and economies. But cancer research has continued to save lives.
In Australia, the overall 5-year relative survival for cancer has increased from 52% to 70% since 1989, making us the global leader in cancer survival. This is largely thanks to public health interventions such as tobacco control initiatives, national screening programs, and investment in cancer research. According to the AAMRI (Association of Australian Medical Research Institutes), medical research yields life-changing health outcomes and savings in the Australian health system, with every $1 invested equating to $3.90 in health benefits.
Over the last 56 years, Cure Cancer has funded 553 projects, many of which have led to global breakthroughs. From the late Prof Pamela Russell AM’s internationally recognised work in producing antibodies against cancer to Dr Arutha Kulasinghe’s discovery of genes that can be used to assess COVID-19 severity in lung cancer patients, emerging researchers continue to make a lasting impact on people’s lives.
These are some of the achievements that have been made possible by supporting the work of emerging cancer researchers:
1. Leveraging spatial mapping technologies

Dr Arutha Kulasinghe's cellular atlas of skin cancer being engulfed by an active immune system.
Spatial biology is a cutting-edge field that is rapidly advancing precision medicine by providing scientists with novel tissue mapping technologies to examine the intricate details of a tumour in 3D surroundings, down to the very molecule and gene. This allows medical experts and specialists to identify cellular structures and visualise areas of therapy resistance for the first time, and gain an understanding of whether a patient will respond well to therapy. It also increases the chances of patients being diagnosed at an early stage of their disease, where prognosis is more promising, and being given the right treatment plan.
Dr Arutha Kulasinghe is a pioneer of this novel tumour mapping approach, considered the ‘most in-depth cellular atlas in the world’, which he is using to assess lung, head and neck, and skin tumour tissues to identify biomarkers for personalised, targeted therapies for patients. In doing so, he and his team, who are based at The University of Queensland, can make individualised assessments of a patient’s tumour and identify biomarkers for immunotherapy, thus making treatment more effective.

“This is like having a Google Map for biology, and the leap in technology is comparable to taking a horse-drawn carriage and turning it into an electric car.”
- Dr Arutha Kulasinghe, 2020 Cure Cancer grant recipient
This year, Dr Kulasinghe has been validating gene signatures in lung cancer through several trials across multiple patients from different demographics. His research has also been significant in treating patients for COVID-19. In a parallel study conducted with Cure Cancer alumnus A/Prof Fernando Guimaraes, they were able to identify a gene signature associated with COVID-19 severity that could also help identify which patients, including those with lung cancer, will need urgent care.
2. Targeting copper in childhood brain cancer

A/Prof Orazio Vittorio's spatial imaging of an immunotherapy drug activating immune cells (in green) to attack tumour cells (in red).
A/Prof Orazio Vittorio, who is based at UNSW Sydney, has also utilised spatial mapping technology to capture the effects of his immunotherapy research on better treatments for childhood cancer, which has already progressed to clinical trials.
Neuroblastoma and glioblastoma are rare and aggressive childhood neuronal cancers for which survival rates are poor, despite the use of intensive therapy. Neuroblastoma accounts for 15% of total childhood cancer deaths and sadly glioblastoma has the worst survival rate of all cancers, with only 5% of children surviving 5 years past their diagnosis.

“As both a cancer survivor and researcher, I always feel an immense pressure to deliver and get the most effective treatments to patients because I know time is of the essence - especially for children in hospitals. Looking at these images, knowing that I am one step closer to improving the lives of patients and increasing their chances of survival, makes me emotional because I have lived through the same experience.”
- A/Prof Orazio Vittorio, 2019-2023 Cure Cancer grant recipient
These tumours are known to ‘feed’ on copper, often having up to six times the normal levels of the metal inside the tumour cells. Through their discovery of the efficacy of targeting copper in brain cancer cells, A/Prof Vittorio and his team have repurposed copper chelating agents (already used for Wilson's disease) that can kill cancer cells with high copper levels and is less toxic than chemotherapy treatments.
Through spatial imaging, A/Prof Vittorio has captured the ‘eureka’ moment when he and his team examined the specific type of immune cells that their newly tested drug stimulated, discovering that these cells were able to initiate an anti-tumour effect by increasing the presence of other immune cells in the tumour mass.
3. Drug discovery and early detection for ovarian cancer

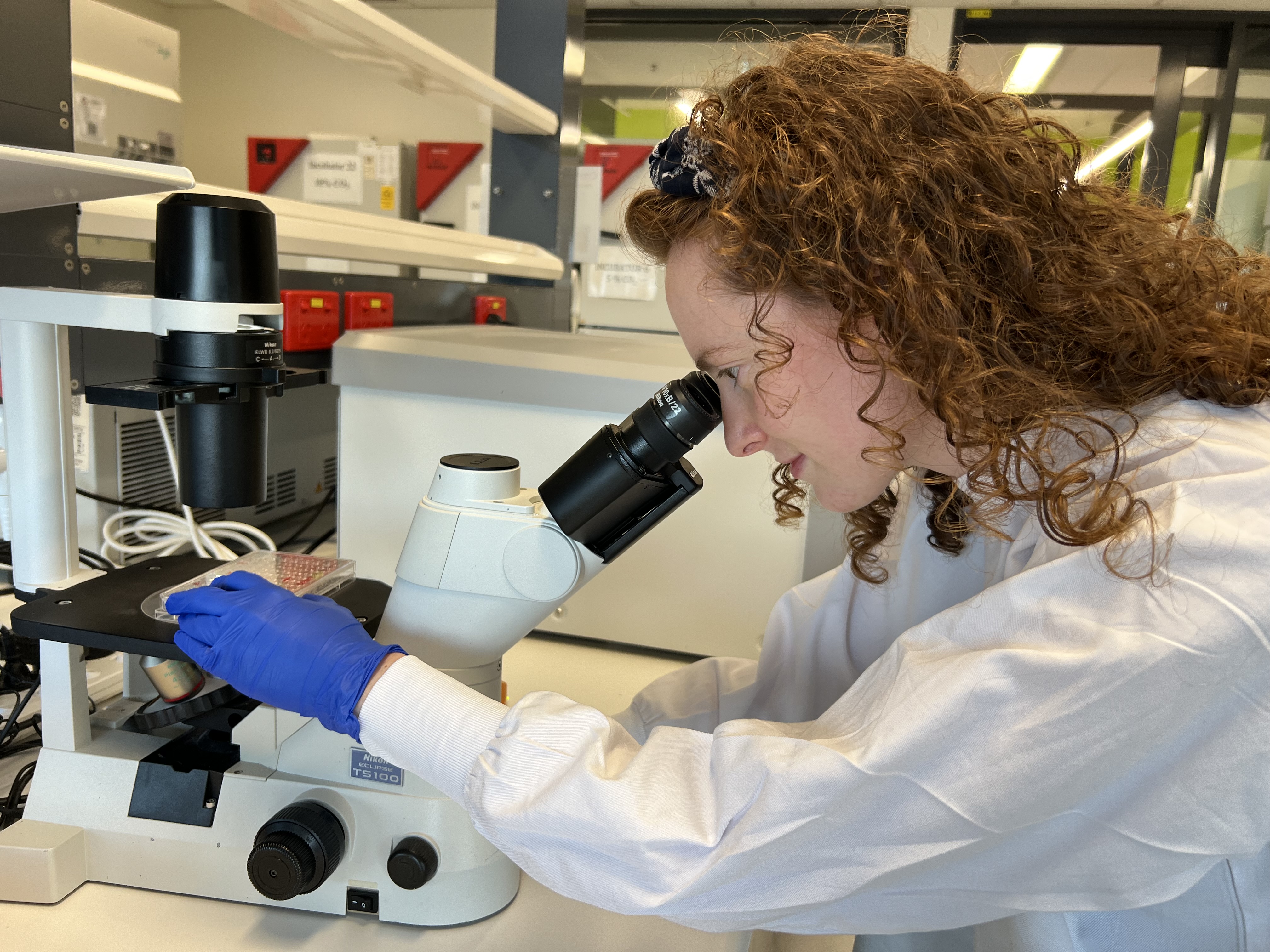
Dr Jessica Holien was a Cure Cancer Researcher of the Year Runner-Up in 2023.
Dr Jessica Holien is a bioinformatics researcher based at RMIT University who is focused on unleashing the power of computers for drug discovery in in mucinous ovarian cancer, a type of gynaecological cancer.
MOC is an understudied subtype of ovarian cancer with terrible outcomes when it is detected at a late stage, or if it recurs. While early-stage MOC patients have a more than 90% chance of surviving the 5 years after diagnosis, patients will typically live between 12 to 30 months if they have metastatic disease. Unfortunately, late-stage MOC is resistant to standard ovarian chemotherapy and new novel therapies are urgently needed since clinicians lack the guidelines for selecting the next treatment to try.
Dr Holien uses high-powered computers to accelerate MOC drug discovery by building cutting-edge computational networks that model how proteins interact in patients’ MOC cells and how they differ from normal cells in healthy individuals. These novel bioinformatic methods have enabled her to identify the proteins whose interactions cause cancer growth. Furthermore, she has used these models to identify and test novel drugs that inhibit these proteins. Her approach offers a faster, more cost-efficient approach to drug discovery, leading to more effective treatment options for patients, whether these are new or repurposed drugs.
“Today the people who inspire me aren’t other researchers, but the patients and supporters I speak to. Their faith in my ability is what pushes me to do all I can to find new treatments for disease.”
- Dr Jessica Holien, 2014 & 2019-2020 Cure Cancer grant recipient
Prof Caroline Ford is Chair of Cure Cancer’s Research Committee and leads the Gynaecological Cancer Research Group (GCRG) at UNSW Sydney, which she established in 2010. Her Cure Cancer-funded research was focused on targeting a new epigenetic therapy for ovarian cancer.
Currently, there is no screening test for ovarian cancer, which is too often detected when it has already spread to other organs, reducing the effectiveness of surgery and treatment. One of Dr Ford’s major ovarian cancer projects at GCRG focuses on developing a reliable screening test for ovarian cancer. By detecting traces of cancer DNA in a patient’s blood at the earliest stage of the disease, this test can help clinicians identify patients who can undergo curative surgery to remove the tumours.

“I have been lucky to meet many amazing people with this disease, but sadly many of these relationships are brief… I’d like to assure ovarian cancer patients that there is an international army of committed ovarian cancer researchers out there collaborating on research and working hard to improve the situation.”
- Prof Caroline Ford, 2011 Cure Cancer grant recipient
4. Creation of more robust models for endometrial and bone cancer

“Their (cancer patients) resilience and fight for survival motivate me to put the same strength into my research, fighting on their behalf, to cure them one day."
- Dr Nathalie Bock, 2020 Cure Cancer grant recipient
One of the main challenges for testing new cancer treatments is the lack of robust models that closely resemble how cancer grows and thrives in the body. This is even more challenging in underfunded cancers such as endometrial cancer (also known as uterine cancer), where there is comparatively less knowledge on how this cancer develops and metastasises.
The typical approach is to grow single cell lines in a petri dish, but this is not the same as how cancer grows in the body. Each solid cancer is like a complex organ, with a 3D structure, consisting of multiple cell types, and with its own microenvironment. As such, it is difficult to predict which therapies will have a real-world impact on patients.
Dr Nathalie Bock, who is based at Queensland University of Technology, is interested in the creation of more robust models in her bone cancer research.
Currently, there are no curative treatments for bone cancer, which often arise when breast and prostate cancer have metastasised in advanced stages of the disease. The only treatments available are typically palliative to help patients with pain management due to poor prognosis.
Dr Bock and her team were able to use tissue engineering, biomaterials and human cells to develop a 3D laboratory model, a ‘mini bone tumour in a dish’, that replicates human bone far more accurately than previous 2D models. They were able to demonstrate that anti-androgens therapies, which are used to treat advanced prostate cancer, may be detrimental to tumours that are found in the bone. This led them to use their miniature models as a drug screening platform for other existing, repurposed, and novel drugs.
5. A new approach to treatment-resistant prostate cancer

Prostate cancer is now the most common cancer diagnosed in Australia, followed by breast cancer. While the 5-year relative survival rate is almost 100% for stage I prostate cancer, at advanced stages of the disease, it reduces dramatically to 36.4%.
Prostate cancer mainly relies on the metabolism of lipids (molecules including fat) in tumours to spread. Despite this, scientists haven’t yet properly explored the role of fatty acid metabolism in the progression of the disease, or its potential as a target for therapy.
The University of Adelaide’s Dr Zeyad Nassar has discovered that fat metabolism, known as fatty acid oxidation, is linked to treatment resistance in prostate cancer as it generates the energy required for cancer cells to proliferate, invade other tissues and resist treatment.
Dr Nassar has identified the important role of the DECR1 enzyme in this process, which is responsible for breaking down polyunsaturated fats (PUFA). In prostate cancer cells, there are higher levels of DECR1 compared to normal cells, and this increases in advanced stages of cancer and cells that have become resistant to therapy.
“Prostate cancer cells use DECR1 not only to generate energy, but to consume PUFA by which cells decrease cell oxidation stress and stay vigorous. Targeting this enzyme using gene-expression modifying techniques decreased prostate cancer cell tumorigenic properties and sensitised them to treatment. As there is no available specific inhibitor for DECR1 yet, we established a collaboration with chemists and drug designers from the University of South Australia. If successful, this will be the first-in-field specific inhibitor for PUFA.”
- Dr Zeyad Nassar, 2019 Cure Cancer grant recipient
These findings laid the groundwork for his successful grant applications at both the national level (Cancer Australia) and the international level (United States Department of Defence), resulting in the acquisition of research funds exceeding $1 million.
Dr Nassar hopes this study will contribute to discovering new treatments and decreasing patient mortality at late stages of prostate cancer when it is known to resist currently available drugs.
6. A legacy that lives on

When reflecting on the achievements of Cure Cancer-funded researchers, we must acknowledge the inspiring legacy of the late Prof Pamela Russell AM, who was the Former Head of Biomedical Imaging and Prostate Cancer Models at Queensland University of Technology and served on Cure Cancer’s Medical Grants Advisory Committee for many years.
A trailblazer for women in STEM, Prof Russell received six grants from Cure Cancer (then the Leo & Jenny Foundation) totalling $175,000 between 1988 to 1996. She was internationally recognised for her work on urological diseases such as bladder and prostate cancer. Her career highlights included the production of monoclonal antibodies against cancer and targeted nanoparticle imaging to improve the diagnosis and staging of prostate cancer.
She published over 200 papers for international journals, numerous books, chapters, and conference papers, and held 2 international and several provisional patents. She collaborated with many other researchers in Australia and overseas, raised over $36 million in competitive grants, mentored 31 postdoctoral scholars, and helped to run 4 international conferences.
"Funding for early-career researchers is absolutely critical in order to allow them to start a career in science or in research, but in particular to help the patients who have cancer."
- Prof Pamela Russell AM, Cure Cancer grant recipient
Beyond her groundbreaking studies, Prof Russell helped to establish organisations that have had a profound impact, including the Prostate Cancer Foundation of Australia, the Australasian Genitourinary Oncology Group, and the Australasian Urological and Prostate Cancer Clinical Trials Group. She was a member of the Australian Prostate Cancer Collaboration and was involved with the Global Action Plan for Movember, bringing together expert clinicians and researchers around the world to make breakthroughs for treating advanced prostate cancer.
Prof Pamela Russell AM’s remarkable life underscores the extraordinary heights that emerging researchers can achieve, and the profound impact they can make on people’s lives when we support and nurture their cutting-edge ideas.
To learn more about emerging researcher successes this World Cancer Research Day, head to Projects and Impacts.