Immunotherapy and precision medicine in breast cancer: Two pioneering projects Cure Cancer is backing
By Alexandra Lapa | 1 October
Every breast cancer is different, yet too often treatments follow a one-size-fits-all path. But what if care could be as individual as the person receiving it? What if doctors could anticipate when a tumour is about to change course, or trigger the immune system to fight back more effectively?
Breast Cancer in Australia
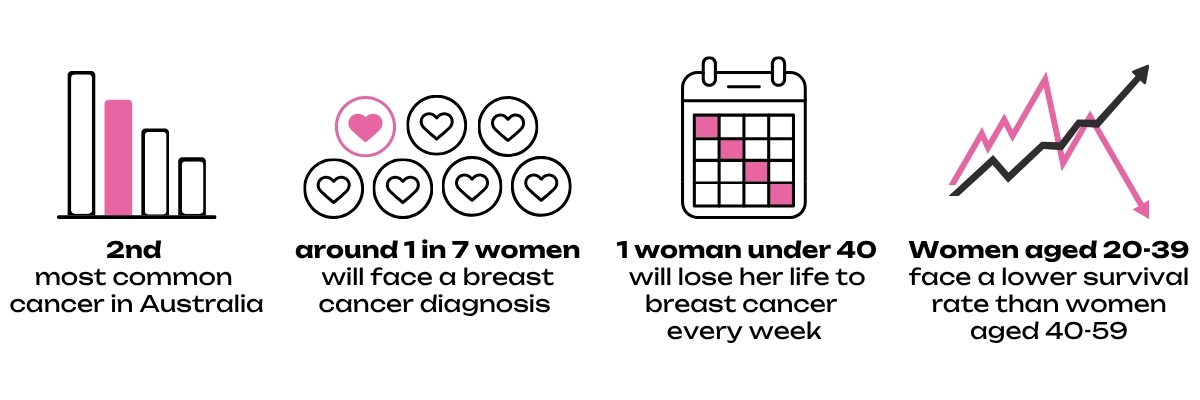
Sources: Cancer Australia, Breast Cancer Network Australia, National Breast Cancer Foundation
This Breast Cancer Awareness Month, we are shining a light on two researchers funded by Cure Cancer who are asking exactly these kinds of bold questions. Their work focuses on two of the toughest challenges in breast cancer today: HER2-positive disease that can learn to resist treatment, and triple-negative breast cancer, which disproportionately affects younger women and offers fewer treatment options.
By reimagining the way we treat these cancers, their projects open the door to a future where care is more precise, more personal, and more powerful.
But first, what is immunotherapy?
Immunotherapy works by turning the body’s own defences into a weapon against cancer. While chemotherapy attacks all rapidly dividing cells with the goal of eliminating cancer cells, immunotherapy helps immune cells recognise which cells are dangerous and target them directly. It is like training the body’s security guards to spot an intruder they used to overlook.
The challenge is that not everyone responds, and some cancers find ways to shut down the immune response. This is why research is vital: to figure out how to expand immunotherapy’s benefits to more people.
Dr Luis Lara Gonzalez: staying one step ahead of HER2-positive breast cancer
“My passion for medical research is deeply personal with two clinician parents and a family that has been touched by cancer. I hope my research will ultimately improve patient outcomes and I believe my generation of onco-bioinformaticians will drive unprecedented change by creating the tools needed for personalised medicine in cancer.”

HER2-positive breast cancer can respond well to treatment at first, but over time some tumours find ways to adapt, eventually becoming resistant and harder to treat.
Dr Luis Lara Gonzalez is studying how HER2-positive tumours change over time and throughout the course of treatment. By measuring the genetic fingerprints of these cancers as they evolve, his study aims to reveal patterns that could one day guide clinicians in practice. Identifying the early signs of resistance may help doctors adjust treatment strategies sooner, keeping therapies effective for longer.
This is one of the first efforts to follow HER2-positive disease longitudinally through large-scale tumour sampling and data analysis, uncovering molecular clues that may help identify the key moments when new strategies, including immunotherapy, could be most effective.
This kind of precision medicine is about moving beyond broad categories and tailoring care to the unique biology of each patient’s cancer. The potential impact is enormous: more time, better outcomes, and treatment plans that feel less like guesswork and more like strategy.
Dr Kellie Mouchemore: making immunotherapy more effective for triple-negative breast cancer
"I am driven by the hope that one day the women in my life won’t have to live with so much anxiety around their risk or diagnosis."
Triple-negative breast cancer (TNBC) is one of the most aggressive forms and more often found in younger women, although rare cases have been seen in men and people of other genders with breast tissue. Standard treatments are limited, and while immunotherapy has brought hope, only some patients benefit.
Dr Kellie Mouchemore is asking why. She is zooming in on TNBC at the level of single cells to understand what is happening inside the tumour’s “neighbourhood.” In some patients, immune cells are shut down before they can attack. By mapping these hidden roadblocks, Kellie is testing ways to remove them so that immunotherapy can succeed in more women.
Imagine being able to flip a switch that allows the immune system to see and attack the cancer instead of being silenced. This research aims to help doctors identify who is likely to respond and expand treatment options for those who currently have very few.
Why this research matters
Both of these projects highlight why investing in emerging researchers is so important. They start with big, patient-centred questions and push into territory that larger grants often overlook.
One seeks to outsmart HER2-positive tumours before they gain the upper hand. The other aims to turn more cases of triple-negative breast cancer into ones that can be treated successfully with immunotherapy. Together, they reflect the kind of daring, high-potential ideas that could transform the future of breast cancer care.
October is Breast Cancer Awareness Month
Awareness matters. But it is research that drives change. Every breakthrough begins with someone asking “what if” and daring to follow where that question leads.
By supporting Cure Cancer, you help brilliant researchers like Dr Luis Lara Gonzalez and Dr Kellie Mouchemore explore new frontiers in breast cancer treatment. Their discoveries may one day give families options that simply do not exist today.
What if the next breakthrough just needs you?