Every day, we lose more than 10 men to male reproductive cancers.
You can change this by helping to fund the breakthrough families are waiting for.

Clint, testicular cancer survivor and Cure Cancer fundraiser
Help improve outcomes for male reproductive cancer patients
Around 1,000 new cases of testicular cancer are diagnosed in Australia every year – in fact, it is the second most commonly diagnosed cancer in young men and people assigned male at birth aged 20-39. For penile cancer, more than 100 new cases of are diagnosed in Australia every year. It is classed as a rare cancer, and the average age of diagnosis is 68.
More than 24,000 new cases of prostate cancer are diagnosed in Australia every year.
Cure Cancer has funded 28 male reproductive cancer research projects so far, but more research is desperately needed. Supporting emerging researchers with the brightest ideas gives us the best possible chance of finding a cure.
Every dollar you donate can make a real difference to our mission. Together, we can cure cancer.
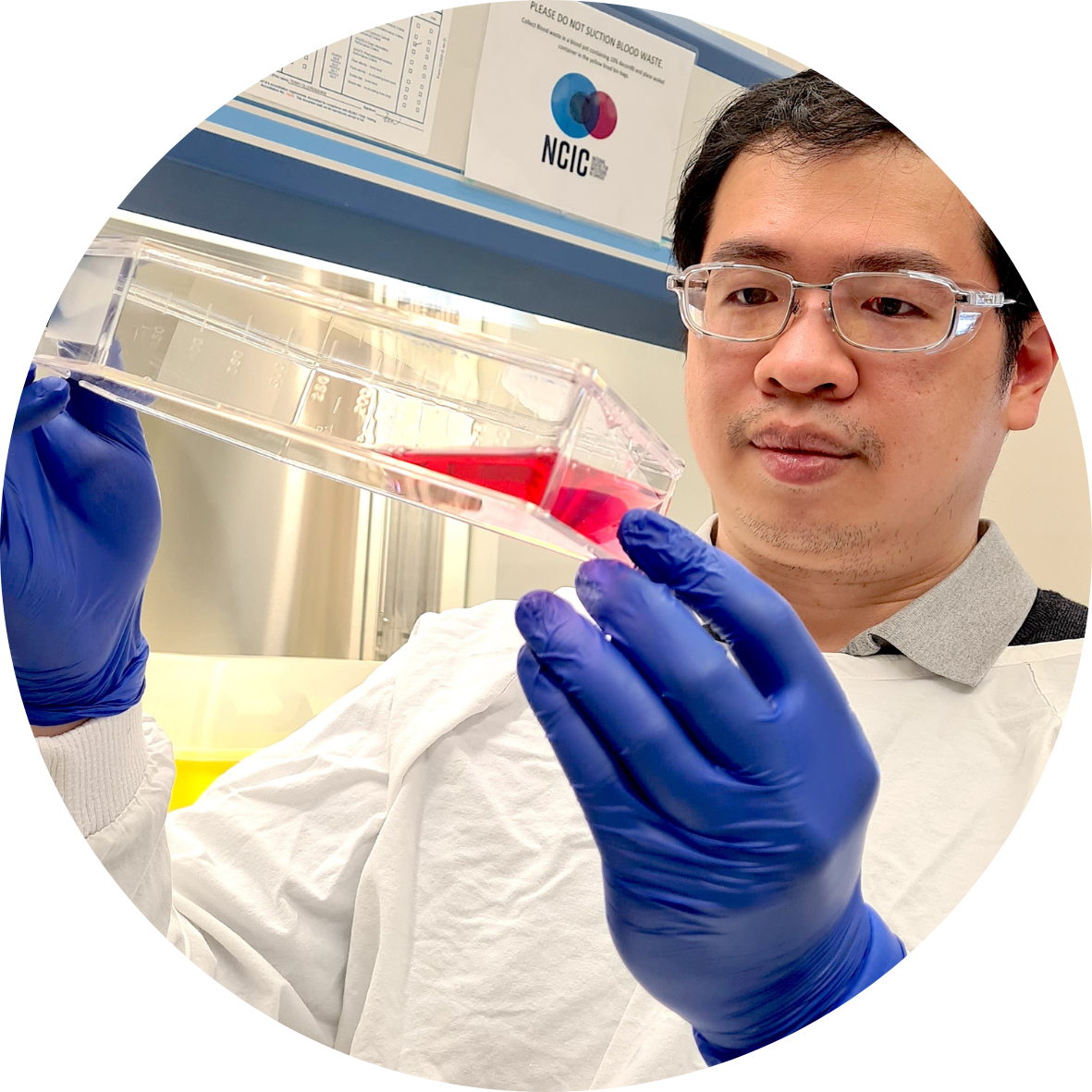
"Male reproductive cancers, including prostate cancer, take a heavy toll on the lives of men, ranking second only to lung cancer in Australia. Your support will help us develop better treatments, offering hope not just to prostate cancer patients but also to those with other male reproductive cancers."
— Dr Eric Kusnadi, Cure Cancer funded researcher
Frequently Asked Questions
What is prostate cancer?
Prostate cancer develops when abnormal cells in the prostate gland grow more quickly than in a normal prostate, forming a malignant tumour. The prostate is a small gland that sits below the bladder near the rectum. It surrounds the urethra, which is the passage in the penis through which urine and semen pass.
More than 24,000 new cases of prostate cancer are diagnosed in Australia every year.What are the types of prostate cancer?
Almost all prostate cancers develop from the cells that line the prostate gland – this type of cancer is called an adenocarcinoma.
What are the common symptoms of prostate cancer?
The most common symptoms of prostate cancer are:
- Problems urinating
- Pain or burning when urinating
- Blood in the urine or semen
- Pain in the back, hips, pelvis or chest
- Weakness or numbness in the legs or feet
- Fatigue and shortness of breath
Your GP will carry out an initial physical examination and discuss your medical and family history with you. They may also perform a rectal examination and carry out a blood test.
If necessary, your GP may then refer you for transrectal ultrasound – where a probe is inserted into the rectum to create a picture of the prostate inside the body. An MRI and biopsy of the tissue may also be carried out. The biopsy results include a Gleason score which will help the doctor to stage the cancer, if cancer cells are present.
Prostate cancer is staged from Stage 1-4.
- Stage 1: Tumour is small and has not spread outside the prostate.
- Stage 2: Tumour is larger but has still not spread outside the prostate.
- Stage 3: The cancer has spread beyond the outer layer of the prostate and may have spread to the seminal vesicles, but not to nearby lymph nodes.
- Stage 4: The cancer has spread to nearby tissues such as the seminal vesicles, rectum or bladder, to nearby lymph nodes, or to distant parts of the body such as the bones.
What is the prognosis for prostate cancer?
The prognosis for prostate cancer varies depending on the stage of the cancer and the person’s overall health.
However, the five-year survival rate is high. Thanks to research, around 96% of patients are still alive five years after diagnosis.
What is penile cancer?
What are the symptoms of penile cancer?
- a growth or sore on the head, foreskin or shaft of the penis
- bleeding from the penis or under the foreskin
- discharge under the foreskin
- a lump or multiple lumps under the foreskin or in the groin
- changes in the colour of the skin on the penis or foreskin
- thickening of the skin on the penis or foreskin
- pain in the shaft or tip of the penis
- swelling at the tip of the penis
- a rash or red skin on the penis
How is penile cancer diagnosed?
What are the treatments for penile cancer?
The main treatments for penile cancer include surgery, radiation therapy and chemotherapy. These can be given alone or in combination. Surgery will involve the surgeon removing the tumour as well as some surrounding healthy tissue. The extent and type of surgery depends on the location, grade and stage of the tumour. In most cases, any physical changes to your penis after an operation can be corrected with reconstructive surgery. Some early-stage penile cancers can be treated with techniques other than surgery, such as laser treatment, photodynamic therapy (PDT), or cryosurgery. You can discuss these options with your medical team.
What is the prognosis for penile cancer?
The prognosis for penile cancer varies depending on the stage of the cancer and the person’s overall health. Your doctor is the best person to advise on your personal circumstances.
What is testicular cancer?
Testicular cancer is male reproductive cancer that develops when abnormal cells in the testicles grow more quickly than in a normal testicle, forming a malignant tumour. The testicles (or testes), are in the scrotum. The scrotum is a loose bag of skin underneath the penis. The testicles make sperm and the hormone testosterone.
Around 1,000 new cases of testicular cancer are diagnosed in Australia every year.
What are the types of testicular cancer?
Most testicular cancer starts in the germ cells, which are the cells that make sperm. The two main types of germ cell cancer are seminomas and non-seminomas. Other types include carcinoma in situ of the testicle and stromal tumours, but these are not as common as germ cell tumours.
What are the common symptoms of testicular cancer?
Testicular cancer can be symptomless. However, common testicular cancer symptoms include:
- Lump or swelling in a testicle
- Change in the size or shape of a testicle
- Build-up of fluid in the scrotum
- Pain or discomfort in a testicle or in the scrotum.
How is testicular cancer diagnosed?
If you are concerned about your health, it’s important to make an appointment with your GP. They will have a chat with you about your medical history and examine the testicles and abdomen for lumps.
If the GP thinks it necessary, you will be referred for an ultrasound to check for tumours in the testicles. Depending on the type of testicular cancer suspected, or if the doctor thinks it may have spread, you may also have X-rays, a computed tomography (CT) scan or magnetic resonance imaging (MRI).
Your doctor will also order blood tests to look for tumour markers in the bloodstream, which can indicate cancer. You may also need a biopsy, which involves a sample of tissue being taken from the testicle for examination under a microscope. However, biopsies are usually avoided for suspected testicular cancer, because the cut through the scrotum can increase the chances of cancer spreading. Results from blood tests and ultrasound are usually sufficient to make a diagnosis of testicular cancer.
Testicular cancer is staged from Stage 1-3:
Stage I: The tumour may or may not have grown outside the testicle. The cancer has not spread to nearby lymph nodes or distant parts of the body.
Stage II: The tumour may or may not have grown outside the testicle. The cancer has spread to at least 1 nearby lymph node but not to distant parts of the body.
Stage III: The tumour may or may not have grown outside the testicle. The cancer has spread to nearby or distant lymphs node and to distant parts of the body such as the lungs.
What are treatments for testicular cancer?
Testicular cancer treatment depends on various factors, including the your test results, the type of testicular cancer you have, whether it has spread, your life stage and your general health
Surgery to remove the affected testicle is common. This is called an orchidectomy. After surgery, your doctor may recommend radiation therapy to kill any cancer cells that may have spread to other parts of the body. If the cancer hasn’t spread, the orchidectomy might be the only treatment that is needed.
If the cancer has spread, chemotherapy may be required, and can also be used to help decrease the risk of cancer coming back after the testicle is removed.
What is the prognosis for testicular cancer?
The prognosis for testicular cancer varies depending on the stage of the cancer and the person’s overall health.
However, the five-year survival rate is high. Thanks to research, around 97% of patients are still alive five years after diagnosis.
How your donation helps

$75
Can help fund an hour of research

$125
Can help fund microscopy imaging to look for immune cells in tumours

$550
Can help fund lab supplies for up to ten vital experiments

$1,000
Can help provide cutting-edge software to analyse cells
Our prostate cancer researchers
Together, we can cure cancer.
Let's stay in touch
To receive updates on our work, campaigns and our impact in cancer research, subscribe to our newsletter.